
-Immunohistochemistry-Paraffin-NBP2-66957-img0002.jpg)
Leptomeningeal enhancement is uncommon but encountered either in isolation or along with cortical lesions (e.g. Deep grey matter and brainstem involvement is more common in children 6. When present, lesions tend to be few in number but sizable, typically bilateral with ill-defined borders. Brain involvementĪcute disseminated encephalomyelitis (ADEM) is a common presenting clinical and imaging phenotype of patients with MOGAD, particularly in childhood 6. In contrast, less than half of adults presenting with MOGAD have brain lesions at the time of diagnosis.
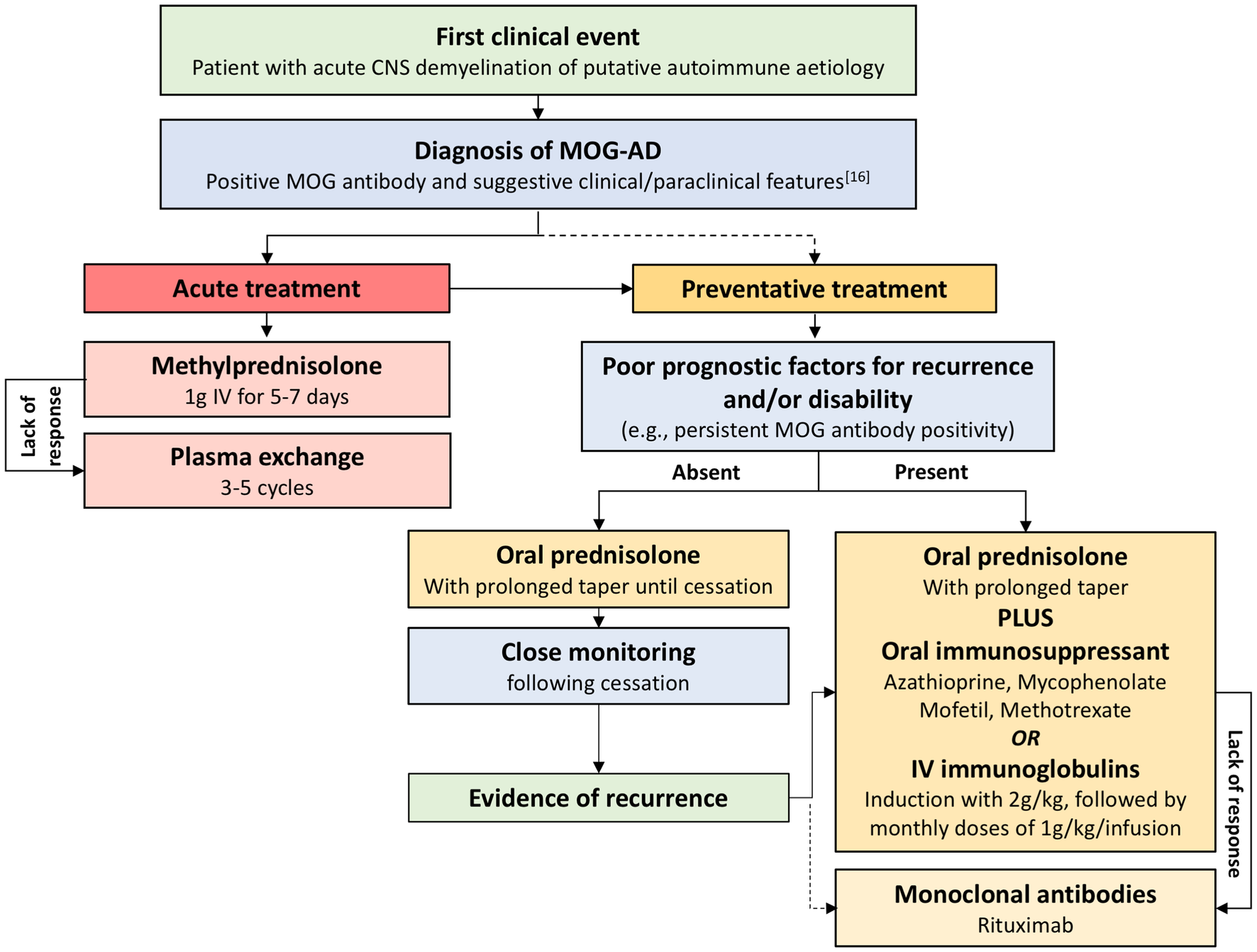
Nonetheless, certain imaging features are increasingly recognized as being more typical of MOGAD, allowing the diagnosis to be suspected on the basis of imaging. acute disseminated encephalomyelitis (ADEM), Neuromyelitis optica spectrum disorder (NMOSD) and to a lesser degree multiple sclerosis). Imaging presentation of MOGAD is variable and with no pathognomonic imaging features, with patients having an imaging phenotype often indistinguishable from other inflammatory white matter diseases of the central nervous system (e.g. Myelin oligodendrocyte glycoprotein is expressed on oligodendrocytes and the outer lamellae of myelin sheaths 6. No specific presentation distinguishes individuals with anti-MOG antibodies from those presenting with similar clinical manifestation but without the antibodies and at the time of writing (2020) no single set of diagnostic criteria are universally accepted 5. seizures - FLAIR-hyperintense lesions in anti-MOG associated encephalitis with seizures (FLAMES) 7Īdditionally, it appears that in approximately half of cases there is viral prodrome 2.longitudinally extensive spinal cord lesions (30%).Not all presentations are equally prevalent, however. International Journal of Ophthalmology Press.Clinical presentation is that of other acquired demyelinating conditions and varies from individual to individual. A broad range of visual field and radiographic findings are identified, a consensus on treatment of neuromyelitis optica spectrum disorders and anti-MOG positive optic neuropathies has yet to be accepted but initial high dose immunosuppression followed by low dose maintenance therapy is favoured.Īnti-aquaporin 4 anti-myelin oligodendrocyte glycoprotein antibody neuromyelitis.

No correlation between initial VA or RNFL and final visual outcome is identified. Visual field testing and radiological findings for each group are described. No correlation was seen for initial RNFL thickness and final visual outcome in this group either. The same statistical analysis was performed for the correlation between retinal nerve fibre layer (RNFL) and VA and similar outcomes were observed. There was no statistically significant correlation (Pearson correlation) between GCL thickness and presenting and final VA. Nine of the 16 patients were female and the average age of onset was 29.2y in the MOG group and 42y in the AQP4 group. Initial and long-term treatment is also summarised.Ī total of 16 patients were included in the study consisting of 12 anti-MOG and 4 anti-AQP4 positive patients. Optical coherence tomography (OCT) scanning was preformed to examine the correlation between ganglion cell layer (GCL) thickness and visual acuity (VA) at presentation and as a determinant of final visual outcome in both groups. Structured clinical exam and multimodal imaging was undertaken sequentially on each. Clinical findings including presence of a relative afferent pupillary defect, colour vision and disc assessment were recorded. Each of these patients had clinical signs and symptoms of optic neuritis and consisted of all patients who had a positive blood antibody result in our centre.

To describe the clinical characteristics and treatments associated with antibody positive optic neuropathies including anti-myelin oligodendrocyte glycoprotein (MOG) and anti-aquaporin 4 (AQP4), alongside diagnostic modalities, investigations, and outcomes.Ī cross-sectional single-centre retrospective case series consisting of 16 patients including 12 anti-MOG positive patients and 4 anti-AQP4 positive patients.


 0 kommentar(er)
0 kommentar(er)
